Diagnosing chronic pelvic pain (CPP) is a complex task that requires a comprehensive, multidisciplinary approach. Healthcare professionals must combine clinical evaluation with imaging tests and specific examinations to obtain a complete picture of each patient’s condition.

Clinical evaluation: Clinical evaluation is the first step in the diagnosis of CPP. It consists of a detailed history and a thorough physical examination. During the history, information is collected about the patient’s medical history, including the onset and duration of pain, triggering factors, pain characteristics, and any previous treatments. In addition, the gynecological, urological, gastrointestinal, and neurological history should be explored. The physical examination includes a visual inspection, palpation of the abdomen and pelvis, and gynecological and rectal examinations. These procedures help identify any physical abnormalities that may be contributing to the pain.
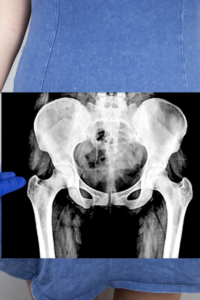
Imaging tests: Imaging tests are essential to visualize internal structures and detect possible causes of CPP. The most common techniques include:
- Ultrasound: Used to evaluate pelvic organs such as the uterus and ovaries. It can detect cysts, fibroids, and other abnormalities.
- Magnetic resonance imaging (MRI): Provides detailed images of soft tissues and is useful for evaluating pathologies such as endometriosis, uterine fibroids, and pelvic inflammatory diseases.
- Computed tomography (CT): Used less frequently, but may be useful in cases where complex abdominal or pelvic pathology is suspected.
- Laparoscopy: Considered the gold standard for evaluating CPP, it allows direct visualization of the abdominal and pelvic cavities. It is particularly useful for diagnosing endometriosis and pelvic adhesions.
Specific examinations: These include laboratory tests and functional tests that complement the clinical evaluation and imaging tests. These may include:
- Blood and urine tests: To detect infections, inflammations or hematological disorders.
- Kidney and liver function tests: To assess organ status and rule out related pathologies.
- Microbiological studies: To identify pelvic or urogenital infections.
- Urodynamic evaluations: Used to analyze bladder and urethral function in patients with urological symptoms.
Challenges in diagnosing DPC

Diagnosing CPD faces several challenges, which can lead to underdiagnosis or misdiagnosis:
Underdiagnosis: CPP is often underdiagnosed due to a lack of recognition of the condition by both patients and healthcare professionals. Many patients with CPP do not seek medical attention due to the normalization of chronic pain or a lack of access to healthcare services. Furthermore, there is a tendency to minimize symptoms or attribute them to psychological causes without a thorough evaluation.
Symptom Variability: The symptoms of CPP can be extremely varied, complicating diagnosis. They may include constant or intermittent pain in the pelvic region, pain during sexual intercourse (dyspareunia), pain when urinating (dysuria), pain during defecation, and referred pain to the lower back or legs. The variability in pain intensity and location, as well as the coexistence of multiple symptoms, can make it difficult to identify the underlying cause.
Comorbidities: CPP often presents with other conditions, such as irritable bowel syndrome, interstitial cystitis, fibromyalgia, and mood disorders. These comorbidities can obscure or complicate the diagnosis, as symptoms may overlap and be misinterpreted as manifestations of a single disease.
Multidisciplinary approaches in diagnosis
Given the complexity and multifactorial nature of CPP, a multidisciplinary approach is essential for an accurate and effective diagnosis. Involving different medical specialties allows for addressing all aspects of the condition and developing a comprehensive treatment plan.
Gynecology: Gynecologists are essential for evaluating gynecological causes of CPP, such as endometriosis, uterine fibroids, and pelvic inflammatory diseases. They perform gynecological exams, ultrasounds, and laparoscopies, and may recommend hormonal or surgical treatments as needed.
Urology: Urologists focus on the urological causes of CPP, including urinary tract infections, interstitial cystitis, and pelvic floor disorders. They perform urodynamic studies, cystoscopies, and kidney function tests to assess the condition of the urinary tract.
Neurology: Neurologists evaluate possible neurological causes of CPP, such as pudendal neuralgia and other neuropathic disorders. They use nerve conduction studies and electromyography to assess nerve function and may recommend specific neuromodulatory or pain-relieving treatments.
Pain Medicine: Pain medicine specialists play a crucial role in the management of CPP, offering both pharmacological and interventional treatments. They assess pain from a comprehensive perspective, considering physical, psychological, and social factors, and work with other specialists to develop a personalized treatment plan.
Fuentes
- Mayo Clinic. Chronic Pelvic Pain: Diagnosis and Treatment. https://www.mayoclinic.org/es/diseases-conditions/chronic-pelvic-pain/diagnosis-treatment/drc-20354371
- ScienceDirect. Diagnosis and management of chronic pelvic pain. https://www.sciencedirect.com/science/article/pii/S0210573X23000138
- NICHD Español. How is pelvic pain diagnosed? https://espanol.nichd.nih.gov/salud/temas/pelvicpain/informacion/diagnostica
- Comprehensive approach to chronic pelvic pain: literature review. http://www.scielo.cl/scielo.php?script=sci_arttext&pid=S0717-75262014000400013

